First things first… force-feeding a human is just not okay. It doesn’t matter how young they are. It is stressful for the child (which decreases their appetite), stressful for the adult, hurts the trusting relationship between adult and child, and all-around is just a bad idea that, frankly, could be considered abuse.
- If you are a parent who is force-feeding: I can only imagine how exhausted, frustrated, and worried you must be. Force-feeding (or even just “tricking” your child into eating something) can break trust and ultimately make progress much more difficult. Please seek an evaluation from a feeding therapist in your area.
- If you are witnessing your child being force-fed by a therapist, caregiver, or other professional: You have the right to say “no.” You are not being unreasonable or rude. There is NO REASON for a professional to force-feed your child and I can only assume that any claim they are making in regard to their ability to treat your child for feeding is totally false. The only explanation for these actions is that they have not been properly educated or trained in anatomy & physiology, sensory needs, oral motor skills, human behavior, or feeding therapy as a whole. Immediate termination of services as well as reporting this person to their licensing board is warranted.
- If you are a professional who is force-feeding: Stop immediately. Seek out proper training. Do BETTER.
End of soap box.
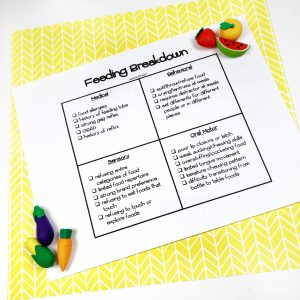
People underestimate the complexities of feeding disorders all too often. I have had too many children come to me who have been in therapy for YEARS with minimal progress. Parents are desperate, children are malnourished, and everyone. is. frustrated. The following are the 4 areas of feeding that must be evaluated and addressed in EVERY CHILD diagnosed with oral phase dysphagia. Heck, let’s go ahead and look at this even if a child is only considered a “picky eater.”
.
.
1. Medical
If a child has any underlying, unaddressed, medical concerns that are related to their feeding, this *must* be addressed first and foremost. Perhaps not before beginning therapy, but it certainly needs to be a top priority.
Here’s what we are looking for:
- food allergies (known or unknown)
- history of (or current) feeding tube
- strong gag reflex
- GERD or history of reflux
Questions to ask during an evaluation:
- What is your child’s favorite drink? (there is a correlation between children who LOVE water/only drink water and reflux)
- How often does your child have a bowel movement? (should be at least once a day)
- What is the consistency of their bowel movements? (should be fluffy- not runny or hard)
- Do they have a current GI or dietician that is following their case?
- Is their pediatrician concerned with their weight?
- Do they have sour breath? (a sign of reflux)
- Do they burp often after eating? (a sign of reflux)
Most of this boils down to this: if the child doesn’t feel good, they are less likely to want to eat or be hungry. Any concerns in this area warrant a call to their pediatrician, a GI referral (preferably one who specializes in children with feeding disorders), and possibly a referral to a dietician.
.
.
2. Behavior
This, in my opinion, is very tricky to sort through. To the untrained eye, every refusal may look behavioral. This is a chicken and the egg situation- we may have behaviors because the kid is so scared of having to eat a food their body can’t handle (for sensory or motor reasons)… BUT in order to work toward our sensory and motor skills… we have to overcome the behavior. It’s enough to give anyone a headache.
Here’s what we are looking for:
- spitting, throwing, or refusing food
- cryings or tantrums at mealtime
- requiring a distractor (i.e. iPad) at meals
- eating differently with certain people or in certain settings
Here’s the big picture: we need to make therapy FUN and break it down into the tiniest steps possible. I used to be very anti-toy/reinforcement during therapy meals but let me tell you… once I embraced the power of 1:1 reinforcers, my kids started making much faster progress AND we were able to quickly fade the toy reinforcers. This trick is helpful even for kids with limited receptive language.
Questions to ask during an evaluation:
- How does your child respond to non-preferred foods?
- How do you feel at mealtimes?
- How does your child feel at mealtimes?
- What does meal time look like at home?
.
.
3. Sensory
Enlist your OTs as needed here. A great way to sort out what sensory issues your kiddo may be fighting through is to take a thorough food inventory and look at patterns. Do they leave out whole categories of food related to temperature, texture, taste, color, shape, size, or smell? If so, food play may be your best friend. When we make it FUN, it’s no longer scary. I made a resource you can find HERE that encourages art projects and silly games and competitions during therapy meals. One pro tip- kids are MUCH MORE LIKELY to interact with a food when they know it’s about to go away. You can employ a cleanup routine to help with this (example: we “kiss our food goodbye” before throwing away).
Here’s what to look for:
- refusing entire categories of food
- limited food repertoire
- strong brand preferances
- refusing to eat foods that touch each other
- refusing to touch or explore a food
Questions to ask during an evaluation:
Basically, get a very very thorough food inventory!
.
.
4. Oral Motor
Having the skills to safely consume foods is critical as well. This is what we’re building up to… but we can’t work on chewing skills if the kid doesn’t allow the food in his or her mouth. Parents often don’t realize their child can’t chew appropriately or lateralize their tongue.
Here’s what we’re looking for:
- poor lip closure or latch
- weak sucking or chewing skills
- overstuffing or pocketing food
- limited tongue movement
- immature chewing skills
- difficulty transitioning from bottle to table foods
Questions to ask during an evaluation:
Don’t rely on a parent interview to give you the information you need here. The priority is for you to look for oral scatter, overstuffing, pocketing, swallowing food whole, and palatal mashing to name a few. Questions that might help:
- Does your child ever have food left over in their mouth after meals?
- Does your child choke while eating? (if liquid- be particularly cautious of aspiration and refer for FEES or MBS) (if solid- check for over-stuffing)
- Get a thorough food inventory. (Leaving out entire categories of foods is another indicator of poor oral motor skills. Foods that require a mature rotary chew include non-processed meats/steak, raw vegetables, fruit with the skin).
- Does your child eat oranges or grapes? (If yes, ask about if they eat it whole or spit the skin back out. If they cannot chew the skin, they may just suck out the juice.)
Tongue thrust may also be present during feeding. If so, you can check out this blog post for further information! If they’re thrusting on foods, they’re probably looking at some articulation therapy as well.
.
.
And there you have it!
Thorough case histories and parent interviews are your friend. Make sure you are watching very closely how the child interacts with foods, chews food, swallows food, and even how they behave after they’ve finished eating. Don’t hesitate to reach out to their pediatrician, nutritionist, previous therapist, or stinkin’ dog walker if you need to. We need the full picture and parents often don’t realize just how important little details can be- so ask ask ask!
For a nice breakdown of the 4 areas of feeding (perfect for a parent handout!) click the image below:
Please feel free to reach out to me with any questions or comments! If you need more support, check out these fun feeding therapy activities! The best way to get a response is to DM me on instagram @SpeechyThings
Thank you for reading!